Two weeks ago we concluded the World Drug Repositioning Congress Europe, a fabulous three-day meeting in London organized by Terrapinn and the first of three major drug repurposing conferences due in 2012. Its transatlantic counterpart – the World Drug Repositioning Congress USA – will take place on December 4-5 in Washington DC. Inbetween, Arrowhead will hold its 2nd Annual Repositioning & Indications Discovery Conference on October 23-24, 2012 in San Francisco. Certainly no shortage of interest in this field! – And we have got new patents for you too: Israeli researchers claim CX-5461, a Pol I inhibitor under development for cancer by a San Diego company, for multiple sclerosis. Good old glycopyrrolate can lower (yes, reduce!) elevated heart rates in COPD patients. And histone acetylase inhibitors can restore impaired endothelial t-PA emergency production in atherosclerosis patients who develop a thrombus.
H.M. Pharma Consultancy will continue to survey the repurposing patent scenery. Please contact us at office@hmpharmacon.com if you need a situation assessed, or a repurposing project designed.
An Anticancer RNA Polymerase I Pathway Inhibitor For Multiple Sclerosis
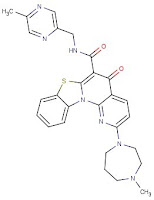 |
| CX-5461 |
Cylene Pharmaceuticals’ CX-5461caused a bit of a stir in the oncology community last July when a paper was published showing evidence that this quinolone-based compound selectively destroys cancer by activating p53 in malignant but not in normal blood cells, an action brought about by the compound’s inhibition of RNA polymerase I (Pol I), a relatively new cancer drug target (Cancer Cell 2012; 22(1):51-65 PubMed). WO/2012/123938(Tel Hashomer Medical Services [IL]; Sept. 20, 2012) builds on the fact that Pol I has a role in the autoimmune response (see e.e., Autoimmunity 2007;40(1):38-47 PubMed) and could therefor be useful in multiple sclerosis. And indeed: in the myelin oligodendrocyte glycoprotein – induced experimental autoimmune encephalomyelitis (EAE) mouse model of MS disease symptoms occurred 10 days later in animals treated with CX-5461 (12.5 mg/kg/day) than in the vehicle-control group, and maximum EAE scores were also much improved. – This appears to be a regular third-party repurposing claim for a compound in preclinical development; if there are corporate connections between Cylene and Tel Hashomer we could not find them through a cursory search.
The Fabulous Glycopyrrolate
On June 21, 2012 the European Committee for Medicinal Products for Human Use adopted a positive opinion for the Seebri® Breezhaler®, as a once-daily inhaled maintenance treatment in adult patients with chronic obstructive pulmonary disease (COPD). The active agent in this inhaler is glycopyrronium bromide, a long-acting muscarinic antagonist licensed to Novartis in April 2005 by Vectura and its co-development partner Sosei. Novartis promptly recoded glycopyrrolate as NVA237 and started a new development line that combined it with indacaterol, creating another investigational inhaler product (QVA149) with blockbuster sales projections. Not bad for an old anticholinergic drug which, in combination with other drugs, was orignally used as an oral and injectable medication to treat intestinal ulcers. This had not been the first repurposing; an oral solution, marketed as Cuvposa®, was approved by the FDA in July 2010 and has been commercially available in the U.S. since April 2011 to treat an orphan condition, chronic severe drooling in children with cerebral palsy. Merz, Inc. acquired Cuvposa from Shionogi Pharma Inc. in August 2012. And now, in WO/2012/120284(Sosei R&D [GB]; Sept. 13, 2012) it is claimed for treating tachycardia — an “unexpected and surprising” claim indeed because it is well known that muscarinic antagonists increase the heart rate. In fact, one of the current key indications for glycopyrronium bromide is for intra-operative bradycardia. However, the trials in COPD patients indicated that at least in this condition glycopyrrolate can slow an excessive heart rate when inhaled in the PowderHale™ formulation of lactose and magnesium stearate. Quite amazing!
New Anticancers and an Old Antiepileptic for Thrombosis
Histone deacetylase (HDAC) inhibitors interfere with the epigenetic control mechanism that helps to unwind nuclear chromatin and makes DNA more accessible to the transcriptional machinery; they generally decrease the transcription rate in nuclei where it is enhanced, and have one obvious application, as cytostatic drugs for cancer. However, HDACs can also act on non-histone proteins, and they can increase production of tissue plasminogen activator (t-PA) in endothelial cells which is a “last line of defense” in thrombosis. This has been described for Trichostatin A and butyrate (Biochem J. 1995;310 ( Pt 1) 171-6, PubMed; Cardiovasc Res 2011; 90(3) 457-63, PubMed). However these substances are not suitable for clinical use due to toxicity and poor pharmacokinetic properties, and hence potential in vivo use was never discussed. In WO/2012/120262(Individuals [SE]; Sept. 13, 2012) the inventors have shown that unexpectedly low concentrations doses of valproic acid (a known HDAC inhibitor) can increase or normalize an inflammation-suppressed t-PA production (a frequent condition in atherosclerosis) by completely off-setting the effects of TNF-alpha. Although this effect is seen with all HDAC inhibitors regardless of their subtype specificity, it is strongest with the hydroxamates (vorinostat, [Merck & Co.’s Zolinza(R)], belinostat[Topotarget / Spectrum Pharmaceuticals], givinostat, panobinostat[Novartis], PCI-24781, JNJ26481585, and SB939) which are pan-HDAC inhibitors.

